Diabetes mellitus is a complex and insidious syndrome characterised by abnormalities in carbohydrate, lipid and protein metabolism.
This may be related to the destruction of special cells in the pancreas (Type 1), or from impaired insulin function, related commonly to obesity and lifestyle factors (Type 2). Type 1 diabetes represents only 10-15% of primary diabetes cases in Australia.
About diabetes
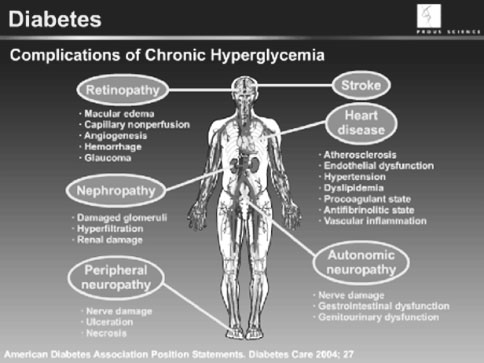
Diabetes can cause extensive disability, poor quality of life, functional impairment and premature death, especially if the disease remains undiagnosed or poorly managed. Diabetes is associated with a range of complications and functional impairment; including coronary artery disease and peripheral vascular disease, stroke, diabetic neuropathy, gangrene leading to amputations, renal failure, male impotence and blindness. Smoking makes these complications worse.