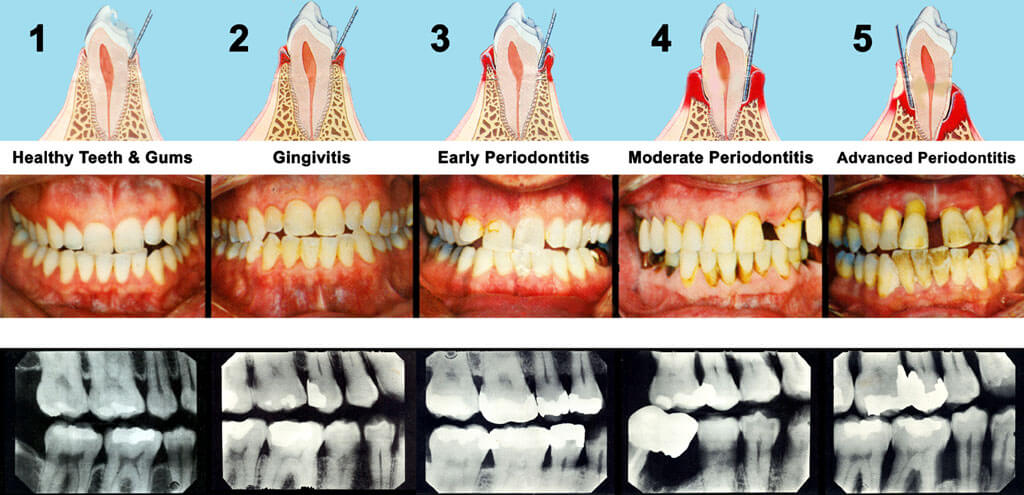
Periodontal (gum) disease is the inflammation and infection of the gums.
It is caused by plaque; a thick and sticky film of bacteria that builds up on the teeth. If the teeth and gums are not cleaned well, or frequently enough, the plaque is left to calcify and becomes hard, cement-like material called calculus, also known as tartar. Your teeth and gums should be examined and cleaned professionally on a regular basis.
Gingivitis
Gingivitis is the milder form of gum disease, which is usually reversible with daily brushing and flossing, and regular cleaning by our dental hygienist. This form of gum disease does not include any loss of bone and tissue that hold teeth in place.
Periodontitis
When gingivitis is not treated, it can advance to periodontitis. In periodontitis, gums pull away from the teeth and form “pockets” that become infected. The body’s immune system fights the bacteria as the bacteria spreads and grows below the gum. Bacterial toxins and the body’s immune system start to break down the bone and connective tissue that hold teeth in place. If not treated, the bones, gums, and tissue that support the teeth are destroyed. The teeth may eventually become loose and have to be removed.